
Fungal infections of the feet begin in the areas between the toes. The infection can later spread to the feet and nail beds. The disease is caused by dermatophytes, molds or yeasts. According to statistics, in our country about 20% of people have foot fungus. The severity of the disease depends on the type of infection, but in any case the disease must be cured, since peeling, severe itching, inflammation and unpleasant odor of the feet cause serious discomfort. We will tell you how to get rid of foot fungus.
What do foot fungus look like?
A fungal infection causes inflammation of the skin where the fungal infection is located. The main types of dermatomycosis of the legs are:
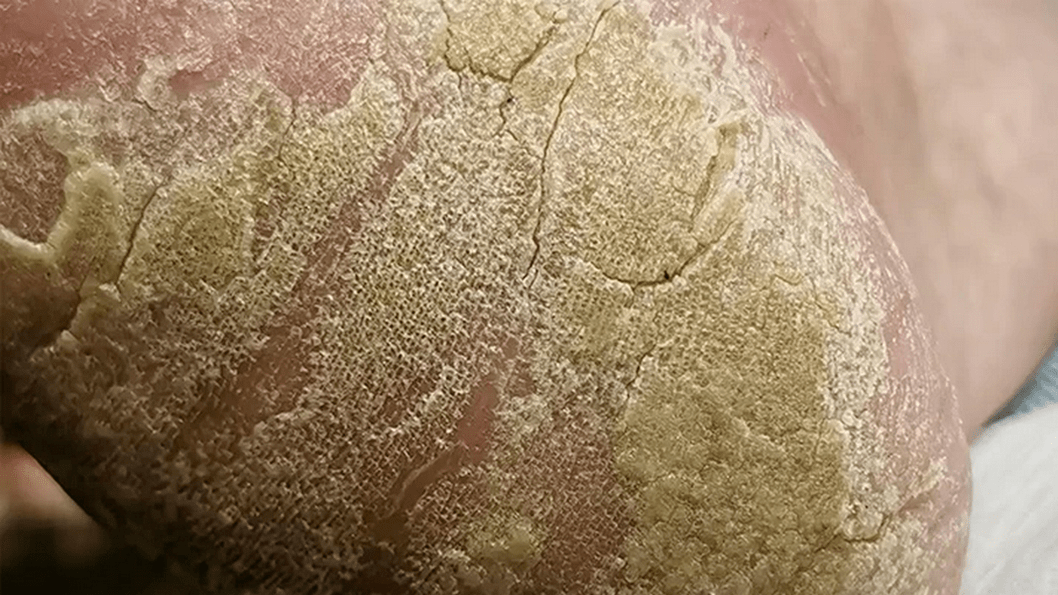
- The fungus on the sole of the foot is scaly, in which the affected area turns red, peels and cracks appear on the skin. The patient often does not feel any discomfort, which contributes to the widespread spread of this type of disease.
- Dyshidrotic foot fungi are located on the arches of the feet, which are not in contact with the ground surface. Small blisters form at the sites of infection, spreading to the inside and outside of the foot, opening and forming erosions and diaper rash on the surface of the skin. The process is accompanied by an itching and burning sensation. After the opening of the vesicles (bubbles), the disease passes into the squamous form.
- A fungus on the skin of the feet that affects the interdigital space is called intertriginous form of the disease and is its most common type. It appears in the form of cracks, the edges of which are covered with a white border of exfoliating epidermis. As a rule, this form has a long-term chronic course and is difficult to treat.
- Shin or ankle fungus appears as round pink or red spots, covered with flakes of skin. As the infection progresses, the inflammation foci grow and the process is accompanied by intense itching.
Onychomycosis
This disease is a type of foot fungus that is characterized by a fungal infection of the nail. You can become infected in showers, saunas, baths and public swimming pools. Scales containing a pathogenic microorganism are quite easily separated from the nail plate and can remain on unpainted floors, carpets, bedding and benches. High humidity allows them not only to survive, but also promotes active reproduction, and therefore the risk of infection increases significantly.
In the initial stage, the infection reaches the epidermis of the feet and causes intense itching. To relieve discomfort, a person begins to comb the infected area, but this only makes the situation worse. Areas of the skin affected by the fungus become covered with small scratches and cracks, microorganisms begin to spread, penetrate under the nail plate, and then begin to multiply uncontrollably.
Serious illnesses such as diabetes or HIV, poor circulation or nail injuries considerably increase the risk of infection.
Onychomycosis is divided into 3 types:

- Normotrophic. With this type of onychomycosis, a change in nail color from normal to yellowish brown is observed. The natural shine, shape of the nail and its thickness remain unchanged.
- Hypertrophic. A final change in the color of the nail occurs, its shine disappears, its shape changes, thickening develops and partial destruction begins.
- Onycholytic. The color of the affected nail changes to brown, becomes thinner and begins to break. His gradual separation from the bed begins. Uneven layers may appear on the exposed part of the nail bed.
Treating this type of fungus on the palms and soles of the hands with topical medications is ineffective because the spores of the fungus are found under the nail. Before starting treatment, the nail must be removed. This is done with the help of keratolytic drugs and patches are also used. In some cases, it is possible to remove the nail mechanically: the dead parts of the nail are cut off with a file or tweezers. It is important to remember that all instruments used must be sterilized.
The combined use of mechanical removal and keratolytic patches is the most effective way to remove diseased nails. As for keratolytic agents, you can use a ready-made kit with a broad-spectrum antifungal drug. It contains a special ointment, files to scrape the nail, and a patch. After the nail plate is removed, you should start taking systemic antifungals: an antifungal drug for systemic use, an oral antifungal agent.

Symptoms
Depending on the form of the disease and the location of the inflammation, the infection is accompanied by different symptoms, with some of the following general signs:
- peeling of the skin;
- mild or severe redness of the skin at the site of the injury;
- itching;
- burning sensation;
- rashes with blisters or cracks on the skin.
Blisters between the toes
The main symptom of athlete's foot, caused by the Candida fungus, is the appearance of blisters between the fingers, usually between the fourth toe and the little finger. The course of the disease is accompanied by swelling of the skin adjacent to the fingers, pronounced areas of redness with small blisters on their surface. The source of inflammation is surrounded by a border of exfoliated epidermis.

dehydrated form
Vesicular fungus or, as it is also called, dehydrated mycosis, is the rarest type of disease. Its main manifestation is numerous vesicles united in conglomerates. Vesicles are bubbles filled with pus or nutrient fluid from the inside. When the fluid begins to turn cloudy, the vesicles burst, leaving ulcers in their place. They begin to merge into a line, forming pronounced scars on the skin. This occurs due to drying and peeling of the skin layers.
Approximately 70% of vesicular fungal infections are accompanied by allergic rashes. A variety of bacteria and viruses begin to penetrate the ulcers. As a result, the disease becomes mixed and identification of the original pathogen becomes more difficult. Therefore, you should consult a doctor as soon as the primary symptoms appear: he will be able to quickly identify the type of foot fungus and start therapy.

Also, this must be done immediately. First of all, before using antifungal drugs, the acute process must be eliminated. It is better to entrust this task to a specialist: he can carefully pierce the vesicles, treat the remaining ulcers with two percent boric acid and apply a bright green or methylene blue solution.
Treatment of advanced disease involves the use of corticosteroid ointments. After eliminating the inflammatory process, it is recommended to use topical antifungal agents. This will suppress the pathogen. We continue to consider the names and types of foot fungus.
First signs
Disease of the skin of the legs is always accompanied by a number of general symptoms, the appearance of which indicates an infection of the skin with spores of harmful microorganisms. You should seek help from a dermatologist in the following cases:
- the appearance of cracks or blisters on the skin in the folds of the feet or between the toes;
- significant thickening and thickening of the skin of the feet;
- redness of skin areas, peeling;
- burning or itching sensation.

Treatment duration
Combined infection of the skin and nail plate requires rehabilitation therapy for one to three months. These terms are considered standard for the most medically effective pharmaceutical products.

Pregnancy requires a lovely visit to the doctor to choose a way to get rid of mycodin infection. Strong medications and therapies that require the use of similar medications are prescribed only under the supervision of a doctor and with strict dosages. Many antibacterial pills that effectively destroy fungi can cause noticeable harm to the fetus. Therefore, whenever possible, during pregnancy, it is recommended that patients be treated with traditional medicine recipes. Many of them allow you to cope with the disease, but provided that the disease has not reached a complex stage. Only classical medicine can help deal with the advanced form.
Modern medications allow you to completely restore the health of your legs within two weeks, provided that signs of infection are detected in time.
Causes
Infection occurs for various reasons after direct or indirect contact of the patient with the carrier of the infection or his personal belongings, household items. Risk factors for getting tinea pedis include:
- leg circulation disorders and related diseases (varicose veins);
- weakened general or local immunity;
- non-compliance with hygiene rules;
- weakening of the body's defense systems after taking antibiotics;
- increased sweating of the skin of the feet;
- presence of minor damage to the skin (abrasions, scratches).
Treatment methods

In most cases, it is possible to completely get rid of a timely detected disease in a maximum of a month. This is a very important point in treatment, since the itching, tissue damage and other manifestations disappear, the patient sometimes suspends treatment, believing that the disease has been defeated. But remnants of the infection can easily cause a relapse.
Treatment should be stopped only with the permission of the doctor and after passing the necessary tests. This is especially true in advanced forms of the disease. The fungus is firmly "fixed" in the body and sometimes it can take at least six months to get rid of it. But the external manifestation of foot fungus in the form of various damage to the skin or nails disappears much earlier, creating the illusion of health. By stopping therapy in this case, the patient will almost certainly cause a relapse.
Treatment of feet with mycoid infection is carried out comprehensively. To get rid of the disease, local antifungal drugs and tablets are used to eliminate the infectious agent that has penetrated the body. To eliminate itching, pain, brittle nails and accelerate tissue regeneration, certain medications can be prescribed. It is not recommended to combine them independently with the main therapeutic group, so as not to provoke an allergic reaction or poisoning of the body due to the simultaneous use of incompatible drugs.
Curing foot fungus at an early stage is quite simple. Two weeks of therapy are usually sufficient to eliminate the symptoms of mycoid infection.
Types of mycoses
Only a dermatologist can accurately determine the type of fungus by visual examination, the data of which is clarified by laboratory tests. Depending on the causative agent of the fungal infection (yeast, mold, fungi of the genus Trichophyton or Candida) on the skin of the feet, there are several main types of the disease, including:
- candidiasis of the feet;
- athlete's foot;
- trichophytosis (or rumbicosis) of the feet;
- onychomycosis (nail fungus).

Prevention
Simple preventive measures will significantly reduce the likelihood of infection. You should only use personal belongings and treat your nails with sterile instruments. When visiting public places, such as baths, saunas, swimming pools, beaches, you must wear your own shoes. By the way, try to choose it in a way that is comfortable for you and allows your feet to breathe. You should worry about prevention ahead of time so you don't have to deal with various types of foot fungus later.
How to deal with
Treatment of fungus on the skin of the legs is a complex long-term therapy, which in severe cases includes the use of systemic oral agents. For minor injuries, emphasis is placed on local therapy with antibacterial and antiseptic agents. In acute forms of the disease, warm baths are prescribed to relieve inflammation and remove dead skin cells. In some cases, it is necessary to treat the patient's shoes and clothing with special compounds to prevent relapses.
System Tools
Systemic oral agents are prescribed in cases of ineffectiveness of local drugs and in severe and advanced forms of the disease. A course of oral antifungal medications is indicated for fungal infections of the deep layers of the skin; They help not only treat the acute stage, but also prevent the disease from becoming chronic. The attending physician selects the dosing regimen, duration of the course and dosage.
Doctors recognize that antifungal medications for systemic use are the best means of systemic treatment of foot fungus. They have an active fungicidal (destroying) and fungicidal (inhibiting the proliferation of bacteria) effect, their active components can accumulate in the upper layers of the epidermis, nails and hair. Before taking it, be sure to read the instructions for use, since these products have contraindications.
Local remedies
Topical drug therapy includes not only the use of antifungal creams and ointments, but also the use of special sprays, lotions, and sprays. The form of the drug is recommended by a dermatologist, depending on the type of causative agent of the infection, the severity of the lesion on the skin of the legs, the stage of the disease and the individual characteristics of the patient's body. The duration of treatment with a local drug can range from 2 weeks to 3 months.
For foot fungus and other forms of mycoses of the skin of the legs, a spray, a suspension for skin application, or a solution for topical use may be prescribed. The products are applied directly to the skin damaged by the fungus or applied to wet swabs soaked in a medicinal solution. All necessary recommendations for use can be obtained from your doctor.
Antifungal ointments
For the treatment of fungus on the skin of the feet, in most cases an antifungal ointment is prescribed, for example a cream with the active ingredient terbinafine hydrochloride or its analogues. Apply the medicine in the form of ointment or cream to the dry skin of the heels or other areas of localization of inflammation, previously carefully cleaned of dead epidermal cells and any other plaque. For different types of diseases, the duration of treatment can vary from 2-3 weeks to 2-3 months.
Experts consider broad-spectrum ointments to be an effective means of combating foot fungus in various forms and stages. The active components of the drug locally fight fungal infection, suppressing the reproduction of its pathogen. The ointment is applied two or three times a day to washed and affected skin for several weeks or months, depending on the degree of damage to the skin.
Home remedies
The use of folk remedies is possible only with the consent of the treating doctor. The main products for baths, compresses and applications against fungus on the skin of the feet are vinegar, propolis, baking soda, decoctions of medicinal plants and laundry soap. The following procedures are practiced:
- Baths with a solution of soda and salt. For 3 liters of water at a temperature of 36-40°C, use 3 tablespoons. l. salt and 3 tbsp. soda. The duration of the procedure is 10-15 minutes, after bathing, rinse your feet with warm water. It is used for acute forms of fungus for 7 to 10 days, twice a day.
- Lotions with herbal decoction. To prepare a decoction, mix dried oak bark, calendula flowers and verbena leaves in equal proportions. To prepare the decoction 3 tbsp. l. pour a glass of boiling water over the mixture and keep on low heat for 10-15 minutes. Make a compress from the resulting decoction three times a day for 20-30 minutes.

erased form
Mycosis of an erased form is almost invisible, its symptoms are minimal. These include: mild itching, burning, mealy peeling, microcracks located in the interdigital areas. If you do not contact a specialist when the first signs of the disease appear, the pathology can progress into the form of onychomycosis, which is much more difficult to treat. In this case, the peeled nail will grow back in one to six months.
Erased mycosis is treated with local preparations: ointments, creams, foams. They allow you to create a layer on the foot that will protect against infection from other infections. It is not recommended to wash your feet for 24 hours after applying this medication.
Only in extreme cases can systemic therapy be prescribed. The problem is that these drugs are toxic and negatively affect some internal organs, such as the liver. Consequently, if the use of local remedies produces any effect, it is better not to take pills.
Infection routes
Fungal spores remain viable in the environment for a long time, so it is easy to become infected with the disease in the most unexpected places. But the most favorable conditions for its development are heat and high humidity. Because of this, people who visit the following are at risk:
- swimming pools;
- Spa;
- saunas;
- gyms;
- Beaches.
Fungus can appear on any object found there, even if regular disinfection is carried out. Therefore, in such places you should avoid common objects and be sure to carry spare shoes.
Military personnel are at risk. Most of the time, army soldiers wear uncomfortable shoes that do not allow air to pass through. Because of this, the feet sweat, microtraumas appear into which the fungus penetrates.
There are two types of infection. The first is the direct path through direct contact with the infectious agent when communicating with a sick person, caring for an animal or walking barefoot on soil and sand. The second, the indirect route, leads to infection through objects belonging to infected people or pets.
Precautionary measures

Preventing a disease is always easier and safer for health than treating it, even using the gentlest method. In the case of a fungal infection, prevention is one of the mandatory rules of life, since it is very easy to get infected. Therefore, to reduce the risk of contracting the disease, it is recommended to follow some simple rules:
- try to eat healthy and eat as healthy as possible;
- do not use other people's things or personal hygiene products;
- use basic protective equipment in public places, such as spare shoes and hygienic antibacterial agents;
- wash your feet and change socks regularly;
- lead a healthy lifestyle;
- Take regular baths to improve foot health;
- Periodically disinfect shoes.
Preventing fungal infection is important not only to prevent it, but also if the disease occurs. In this situation, compliance with sanitary and hygienic rules helps to accelerate healing and prevent infection of other people with the fungus.
















